High Cortisol Levels: Symptoms, Causes, and When to Seek Help by nutritionist Laiba Imran
High Cortisol Levels: Symptoms, Causes, and When to Seek Help
As a nutritionist, I often see clients experiencing health issues linked to stress and hormone imbalances. One of the most important hormones in this conversation is cortisol. While it’s normal for cortisol levels to rise and fall throughout the day, consistently high cortisol can harm your health. Doctors call this Cushing’s syndrome or hypercortisolism.
Let’s look at the symptoms, causes, and when to see a doctor, along with some nutrition insights.
Symptoms of High Cortisol
High cortisol can show up in different ways, and the intensity often depends on how long your levels have been elevated. Here’s what to look out for:
-
Weight gain – Often noticeable in the face (creating a “moon face” look), upper back (between the shoulder blades), and abdomen. Unlike typical weight gain, this happens relatively quickly, even without major dietary changes.
-
Acne and skin issues – Breakouts are usually inflammatory and can appear on the face, chest, or back. Skin may also feel oilier than usual. At the same time, skin becomes thinner and heals slowly, leading to easy bruising.
-
Facial flushing – A reddish, flushed appearance across the cheeks.
-
Muscle weakness – Especially in the upper arms and thighs, making everyday tasks (climbing stairs, lifting groceries) more difficult.
-
Severe fatigue – Feeling drained despite adequate sleep, often paired with brain fog and difficulty concentrating.
-
Mood changes – Irritability, restlessness, or even anxiety and low mood.
-
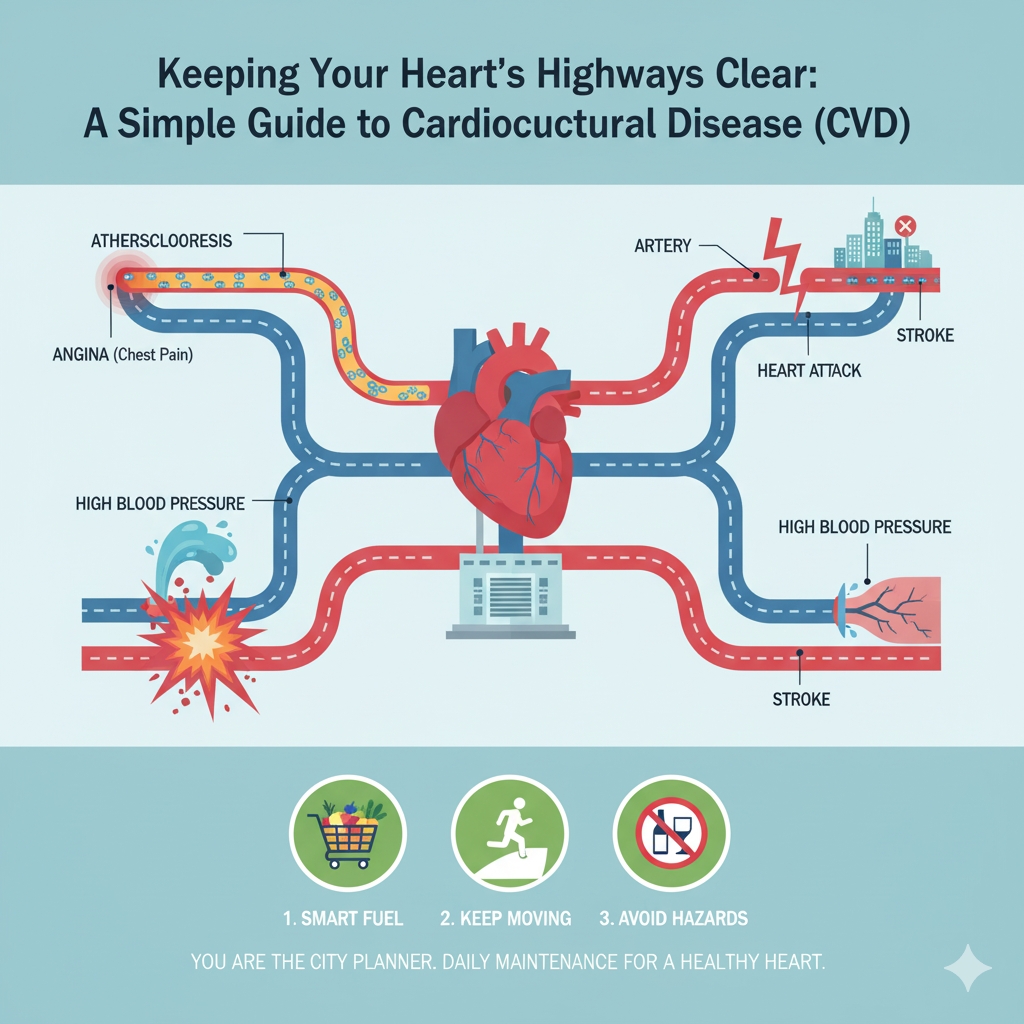
Headaches – Linked to elevated blood pressure and tension from chronic stress.
-
Other changes – High blood pressure, poor wound healing, and in some women, unwanted facial or body hair (hirsutism).
Causes of High Cortisol
Your adrenal glands release cortisol under the direction of your brain (hypothalamus and pituitary gland). When this system is overstimulated, cortisol production can go into overdrive. Common causes include:
Chronic Stress
The body’s “fight-or-flight” response raises cortisol. In modern life, stress may come from work, finances, relationships, or lack of sleep.
Unlike short bursts of stress, chronic stress keeps cortisol high, affecting metabolism, weight, and immunity.
Pituitary Gland Problems
Tumors (usually benign) in the pituitary gland can lead to excess ACTH production, signaling the adrenal glands to release too much cortisol.
Adrenal Gland Tumors
Tumors (benign or malignant) in the adrenal glands may secrete excess cortisol directly. These can sometimes cause abdominal discomfort if large.
Medication Side Effects
Long-term use of corticosteroids (like prednisone, hydrocortisone, or dexamethasone) can mimic the effects of high cortisol.
Stopping corticosteroids suddenly is dangerous—always taper under medical guidance.
When to Contact a Doctor
If you notice several of these symptoms—particularly rapid weight gain in the face or belly, stubborn acne, muscle weakness, or extreme fatigue—it’s important to consult a doctor.
Doctors may recommend:
-
Blood, saliva, or urine cortisol tests to measure hormone levels.
-
Imaging (MRI or CT scans) to look at the pituitary or adrenal glands.
High cortisol increases your risk of heart disease, osteoporosis, and diabetes, so early detection is key.
Nutritionist’s Perspective: Supporting Cortisol Balance
While medical treatment is essential for Cushing’s syndrome, nutrition and lifestyle also play a role in managing stress-related cortisol elevations.
-
Stabilize blood sugar → Eat balanced meals with lean proteins, healthy fats, and complex carbs (e.g., salmon with quinoa and vegetables). Skipping meals or eating sugary snacks causes blood sugar crashes that trigger cortisol release.
-
Support skin health → Vitamin C (citrus fruits, kiwi, bell peppers) supports collagen, helping with skin healing and acne. Zinc-rich foods (pumpkin seeds, chickpeas) aid skin repair.
-
Anti-inflammatory foods → Omega-3s (walnuts, flaxseeds, fish) can reduce inflammation linked to cortisol.
-
Limit stimulants → Too much caffeine or processed sugar worsens cortisol imbalance.
-
Hydrate → Dehydration itself is a mild stressor that raises cortisol.
Takeaway
High cortisol is more than just “stress.” It can cause noticeable weight gain, stubborn acne, fatigue, and muscle weakness. Causes range from stress to medical conditions like pituitary or adrenal tumors.
If you suspect high cortisol, see a doctor for proper testing. Alongside medical care, a balanced diet, regular movement, good sleep, and stress management strategies are powerful tools for supporting hormone balance.